Allergy Services for Primary Care Physicians: Expanding Access to Long-Term Allergy Relief
Allergies affect more than 100 million people each year. Yet despite their widespread impact, allergies often go untreated due to the scarcity of specialist care. That’s why United Allergy Services is focused on introducing allergy treatment and immunotherapy to primary care practices—the first and often only point of contact for patients suffering from allergies. Let’s look at how UAS is making allergy care part of primary care.
Allergies are among the most common chronic conditions in the United States. Yet, despite the prevalence of food and environmental allergies and the associated health complications—including allergic asthma, sinus infections, and even anaphylaxis—many patients never receive proper diagnosis or treatment. Instead, they rely on over-the-counter medications that only mask symptoms rather than addressing the root cause.
Allergy Care Is Primary Care
Primary care physicians (PCPs) are often the first and only point of contact for patients suffering from allergies. By incorporating allergy testing and immunotherapy into their practice, PCPs can offer their patients a comprehensive, long-term solution, without the need for frequent specialist referrals. Allergy immunotherapy is the only treatment proven to modify the immune response to allergens, providing lasting relief rather than temporary symptom control.
United Allergy Services: Bringing Allergy Testing & Treatment to PCPs
United Allergy Services (UAS) partners with primary care providers to offer in-office allergy testing and customized immunotherapy treatment, enabling them to expand their scope of care with minimal additional workload. Since 2009, UAS has successfully partnered with over 2,500 practitioners across more than 20 states.
How UAS Supports PCP Practices
UAS offers two models for PCPs: a UAS-staffed Allergy Center or a self-managed Testing & Immunotherapy Kit package.
The UAS Allergy Center is fully supplied, staffed and managed by UAS. It is designed to integrate seamlessly into the practice with minimal disruption or outlay. This program includes:
- Clinical Allergy Specialists (CAS): Trained, onsite professionals who educate patients, conduct allergy testing, and coordinate immunotherapy.
- Comprehensive Food and Environmental Allergy Testing: Identifies sensitivities to pollen, dust mites, mold, and pet dander as well as certain foods (e.g. peanuts, lactose).
- Custom Immunotherapy Plans: Based on proprietary protocols, personalized allergy treatment options include subcutaneous (allergy shots) and sublingual (allergy drops) to maximize patient convenience and adherence.
- Full-service Supply & Compliance Management: UAS handles all allergy center supplies, from test extracts to patient education materials, ensuring a seamless experience.
- Insurance & Billing Support: Our team assists with reimbursement processes, making allergy services accessible and affordable for both patients and practices.
With the UAS Testing & Immunotherapy Kits, practices can enhance patient care while maintaining flexibility in how allergy services are incorporated. The Kit option includes:
- Environmental Allergy Testing Kit: Screens for 54 regionally relevant allergens, including trees, grasses, weeds, molds, and pet dander.
- Food Allergy Testing Kit: Identifies sensitivities to 23 common food allergens with panels tailored for adult and pediatric patients.
Both kits include personalized subcutaneous or sublingual immunotherapy options through UAS’s prescription-based formulations.
The Value of Experience
United Allergy Services has an unequalled record of success in delivering effective allergy treatment:
- UAS has more patients on our protocol than any other allergy service provider in the United States.
- We have partnered with more than 2,500 providers in 20+ states to provide allergy testing and immunotherapy services.
- Since 2011, UAS has conducted over 575,000 allergy and food sensitivity tests and served over 350,000 patients with 36+ million immunotherapy treatments in our allergy care clinics.
Enhancing Allergy Care in Primary Practices
With limited access to allergy specialists, many allergy sufferers and their doctors are forced to rely on medications that only mask allergy symptoms, increasing the risk of patients developing long-term respiratory conditions such as asthma.
By partnering with United Allergy Services, primary care practices are able to provide convenient, in-office testing for the full range of allergies and food sensitivities along with safe, well-proven immunotherapy.
Patients enjoy dramatic improvements in quality of life while PCP practices achieve higher levels of patient care and overall satisfaction.
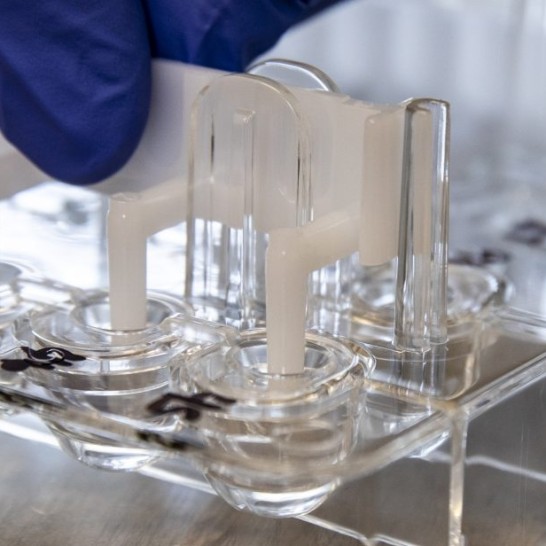
United Allergy Services Featured in Fujitsu Case Study
We are happy to share that United Allergy Services was recently featured in a Fujitsu case study highlighting how we achieve precise inventory tracking and process automation to enhance patient safety and efficiency. The case study explores how UAS leverages Fujitsu’s GLOVIA® OM solution, in conjunction with Salesforce, to improve the allergy care services we offer through our provider partners.
How UAS Improved Efficiency and Operational Care with GLOVIA® OM
As a leading provider of allergy testing and immunotherapy solutions such as allergy shots and allergy drops, UAS partners with healthcare providers to deliver effective and personalized allergy care. Managing thousands of patient interactions daily requires a robust and scalable system that ensures accuracy, compliance, and efficiency.
To help address these needs, UAS implemented GLOVIA® OM, a solution from Fujitsu designed to optimize data management and logistics. This system has improved the way we manage and track inventory, and helps ensure patient safety and regulatory compliance, leading to:
- Improved operational efficiency and patient care
- Optimized patient safety with precise inventory tracking
- Automated reorder process allowing clinics to focus on patient care
Mary Ellen Ault, Senior Director of Technology Services at UAS, stated, “We needed a very detailed and robust data structure to manage the tracking of antigens and extracts used in allergy tests and treatments. The inventory management piece of it is extremely important for us because we track down to the lot detail.”
A Partnership Driving Better Healthcare Outcomes
Leveraging Fujitsu’s GLOVIA® OM solution underscores our commitment to utilizing advanced technology to deliver high-quality ancillary medical services while ensuring seamless provider workflows. This technology has helped us scale our services efficiently, empowering our partner providers to focus on what matters most—delivering the best possible care to allergy sufferers.
We invite you to read the full case study to learn more about how UAS is utilizing cutting edge technology to revolutionize allergy testing and immunotherapy treatment.
Allergy Testing Kits & Immunotherapy from UAS: A Flexible Solution
Adding allergy care allows healthcare providers to address a common patient need and create a new income stream within the existing framework of their practice. However, we know that every medical practice has different requirements. For practitioners looking to integrate allergy testing and treatment without committing to a fully staffed and supplied UAS allergy center, we offer a flexible alternative: allergy testing kits and immunotherapy.
Expanding patient services with ancillary offerings such as allergy testing and immunotherapy is an effective way for medical practices to counter the stiff financial headwinds many are facing. Adding allergy care allows providers to address a common patient need, improve satisfaction, and create a new income stream, all within the existing framework of their practice.
However, every practice operates differently, with unique workflows, staffing models, and space considerations. For providers looking to integrate allergy testing and treatment without committing to a fully staffed and supplied UAS allergy center, we offer a flexible alternative. UAS Allergy Testing Kits & Immunotherapy enables practices to incorporate in-house allergy care while maintaining operational efficiency and clinical control.
Allergy Testing Kits Designed for Clinical Flexibility
UAS offers comprehensive allergy test kits for both environmental and food allergy testing, equipping providers with everything needed to administer skin prick allergy tests in-office. Each allergy testing kit includes test materials, patient education resources, and virtual training to ensure staff readiness. Ongoing customer support is available for clinical guidance, operational questions, and prescription fulfillment.
- Environmental Allergy Testing Kit: Screens for 54 regionally relevant allergens, including trees, grasses, weeds, molds, and pet dander.
- Food Allergy Testing Kit: Identifies sensitivities to 23 common food allergens with panels tailored for adult and pediatric patients.
Comprehensive Immunotherapy Options
Practices offering allergy treatment can provide personalized immunotherapy through UAS’s prescription-based formulations:
- Subcutaneous Immunotherapy (SCIT): Allergy shots available in single or dual-vial sets for long-term symptom relief.
- Sublingual Immunotherapy (SLIT): Allergy Allay Drops® offer a convenient, at-home alternative to injections.
A Scalable Approach to Allergy Care
With the UAS Allergy Testing Kits & Immunotherapy, practices can expand their services in a way that aligns with their needs—whether through occasional in-office testing or a more structured allergy treatment program. This solution allows providers to enhance patient care and practice growth while maintaining flexibility in how allergy services are integrated.
For more information on how the UAS Allergy Testing Kits & Immunotherapy can fit into a practice, contact United Allergy Services.
Pediatrics: How Early Allergy Testing & Treatment Can Benefit Young Patients
Allergies are a common yet often overlooked concern in pediatric care, affecting millions of children across the U.S. While allergy symptoms like sneezing, itchy eyes, and congestion may seem minor, untreated allergies can lead to more serious conditions, including asthma, chronic sinus infections, and sleep disturbances.
Early allergy testing and treatment can significantly improve a child’s quality of life, preventing unnecessary discomfort and long-term health issues. United Allergy Services (UAS) partners with pediatricians to provide in-office allergy testing and immunotherapy, ensuring children receive timely and effective care.
For pediatricians, adding allergy testing and treatment services to their practice offers clinical benefits for young patients and provides a valuable opportunity to enhance their scope of care with ancillary medical services.
Common Pediatric Allergy Symptoms
Identifying allergies in children can be challenging since symptoms often mimic those of colds or respiratory infections. Parents and healthcare providers should be aware of key indicators such as:
- Persistent nasal congestion or sneezing
- Itchy, watery eyes
- Skin reactions, including eczema or hives
- Frequent ear infections or sinus infections
- Coughing, wheezing, or shortness of breath
- Sleep disturbances due to congestion or postnasal drip
Common Triggers
Children’s allergies often stem from seasonal allergens like pollen, as well as perennial allergens such as:
- Dust mites
- Pet dander
- Mold spores
- Certain foods (though UAS treats only environmental allergies)
As previously noted, without proper diagnosis and management, allergies can lead to more severe conditions, including asthma and chronic respiratory issues.

The Importance of Early Allergy Testing
Research shows that early allergy testing and treatment can prevent the progression of allergic rhinitis into asthma. According to the Preventive Allergy Treatment (PAT) study, 45% of untreated children developed asthma over 10 years, whereas only 25% of children who received allergen immunotherapy (AIT) developed asthma. Early identification allows for targeted intervention, helping children avoid unnecessary medications, frequent doctor visits, and reduced quality of life due to persistent symptoms.
How Pediatric Allergy Testing Works
United Allergy Services offers in-office skin prick testing, which is:
- Safe – Designed specifically for children, non-invasive, and physician-supervised
- Efficient – Identifies common environmental allergens within a single visit
- Accurate – Provides a clear picture of a child’s specific sensitivities, enabling a personalized treatment approach
Treatment Options & Benefits of Early Intervention
Once allergens are identified, families can choose from several treatment options:
1. Allergen Avoidance Strategies
- Reducing indoor allergen exposure (e.g., air purifiers, hypoallergenic bedding).
- Implementing seasonal precautions, like keeping windows closed during peak pollen times.
2. Medication Management
- Non-drowsy antihistamines, nasal sprays, and leukotriene inhibitors can help manage symptoms but do not address the root cause.
3. Immunotherapy
Unlike symptomatic relief medications, allergen immunotherapy (AIT) builds long-term tolerance by gradually desensitizing the immune system to allergens.
- Subcutaneous Immunotherapy (SCIT): Administered via injections under the provider’s supervision.
- Sublingual Immunotherapy (SLIT): Allergy drops placed under the tongue for at-home administration.
The Proven Benefits of AIT in Children
- Reduces symptoms of allergic rhinitis and asthma
- Decreases the likelihood of developing new allergies over time
- Lowers long-term healthcare costs by reducing medication dependence and emergency visits
- Prevents progression from allergic rhinitis to asthma
Studies have shown that pediatric patients who undergo immunotherapy experience lasting allergy symptom relief even years after stopping treatment.
Enhancing Pediatric Care with Allergy Services
Many children with allergy-related conditions visit pediatricians first. By integrating allergy testing and treatment, pediatricians can:
- Improve patient outcomes – Address allergies at their source rather than just treating symptoms
- Provide comprehensive care – Reduce the need for specialist referrals while managing allergies in-house
- Support long-term respiratory health – Prevent complications like asthma and chronic sinus issues
The United Allergy Services Advantage for Pediatricians
UAS provides a seamless, physician-supervised allergy program tailored for pediatric practices:
- Customized Immunotherapy: Personalized treatment plans based on each child’s allergy profile.
- In-Office Allergy Testing & Treatment: Delivered within the pediatrician’s practice, improving accessibility for families.
- Convenience for Families: Allows children to receive care from a trusted provider in a familiar setting, with at-home immunotherapy options available.
- Proven Safety & Efficacy: UAS analyzed the systemic reaction rate of 15,000 pediatric patients, six to 17 years of age, using the physician-approved proprietary UAS immunotherapy protocol. Out of that population, a total of 10 patients experienced systemic reactions, all of which were very mild (grades 1 to 2). This represents a reaction rate of 0.06% in pediatric patients. (Reported literature of systemic reactions by allergists is between 3-7% for all age groups.)
Adding UAS allergy services helps pediatricians expand their practice offerings while ensuring high-quality, evidence-based allergy care.
Conclusion
Allergies are more than just a seasonal nuisance. They can impact a child’s health, development, and overall well-being. Early allergy testing and immunotherapy can significantly reduce symptoms, prevent the progression of allergic diseases, and improve long-term outcomes.
For parents, now is the time to consider early allergy testing for children experiencing persistent allergy symptoms. For pediatricians, integrating UAS’ in-office allergy program is an effective way to enhance patient care, improve clinical outcomes, and provide families with accessible, long-term allergy solution.
The Primary Care Practice Crisis: It’s Time to Play Offense
In an article published in Medical Economics, Brad J. Scoggins, FO, DAAP contends that it’s not enough for medical practices to counter adverse market forces by cutting costs and streamlining operations. He argues that practices must take steps to generate more revenue—specifically by offering embedded services from an established specialist provider.
 The primary care practice crisis: It’s time to play offense. That’s the title of a timely article written by Brad J. Scoggins, FO, DAAP. His thesis: “When primary care practices are being strangled by market forces beyond their control, the fastest way to counter those forces is to quickly generate more revenue.“
The primary care practice crisis: It’s time to play offense. That’s the title of a timely article written by Brad J. Scoggins, FO, DAAP. His thesis: “When primary care practices are being strangled by market forces beyond their control, the fastest way to counter those forces is to quickly generate more revenue.“
Scoggins is one of United Allergy Services’ newest allergy partners, and he uses that experience as the proof of his argument that the fastest way to ramp up revenue is by “. . . offering embedded clinical services from an established specialist partner . . . that can be integrated into the practice’s clinical, operational and financial workflows.”
“It is hard to miss the headlines about the unprecedented challenges threatening family and internal medicine across the primary care spectrum,” Scoggins writes. “This traditional and essential gateway to health care in the United States is buckling due to:
- Crushing administrative burdens from payers
- Accelerating costs exacerbated by inflationary pressures
- Anemic reimbursement rates that don’t keep pace with the first two threats
- Corporate competitors like Amazon and CVS blurring the primary care sector for patients
Scoggins acknowledges that “playing defense” against such threats is essential and that most practices are doing everything they can to streamline workflows, leverage technology, manage costs, and negotiate the best possible contracts with payers.
However, these defensive tactics don’t address one of the biggest issues facing providers: patient leakage. According to Scoggins, “It is common for primary care practices to refer patients out for services that they don’t offer, along with the revenue those treatments represent. Patient leakage due to referrals . . . is a key cause of stress on independent and large group primary practices alike.”
The solution, he says, is to recapture those referrals. “Assuming a practice is effectively delivering all the routine core primary care treatments and services, it is time to expand into ancillary medical services and the additional revenues and other benefits they represent.”
As mentioned, Scoggins focuses on allergy testing and treatment “. . . as an opportunity for primary care practices to diversify services, meet growing patient demand, keep patients within the practice, and generate substantial new revenue.”
As Scoggins notes, “Primary practices that are offering ancillary allergy services to their patients are not only capturing a larger share of patient health care spend and alleviating reimbursement pressures, but on average a practice could consistently generate an additional $150,000 to $250,000 yearly (based on practice size and payer mix). Oftentimes, that revenue range is equivalent to what an additional physician could produce for the medical practice, but with a much smaller footprint and administrative cost.”
Ready to review the full article?
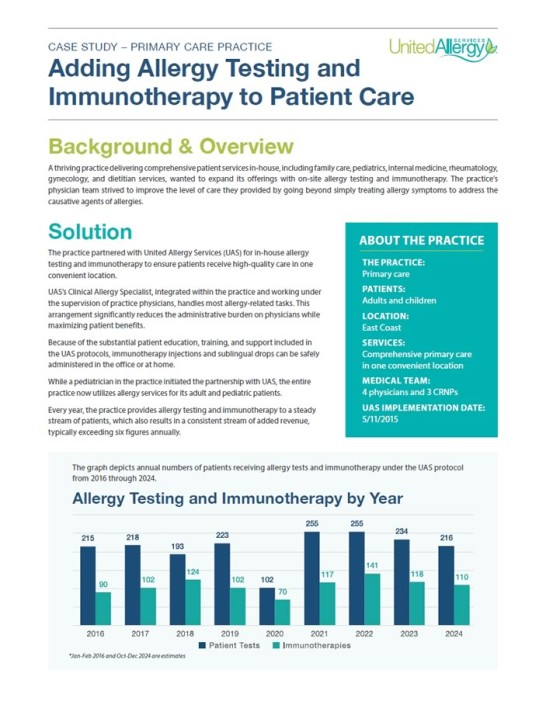
Case Study: Adding Allergy Testing and Immunotherapy to Patient Care
A thriving practice delivering comprehensive patient services in-house, including family care, pediatrics, internal medicine, rheumatology, gynecology, and dietitian services, wanted to expand its offerings with on-site allergy testing and immunotherapy. The practice’s physician team strived to improve the level of care they provided by going beyond simply treating allergy symptoms to address the causative agents of allergies.
Solution
The practice partnered with United Allergy Services (UAS) for in-house allergy testing and immunotherapy to ensure patients receive high-quality care in one convenient location.
UAS’s Clinical Allergy Specialist, integrated within the practice and working under the supervision of practice physicians, handles most allergy-related tasks. This arrangement significantly reduces the administrative burden on physicians while maximizing patient benefits.
Because of the substantial patient education, training, and support included in the UAS protocols, immunotherapy injections and sublingual drops can be safely administered in the office or at home.
While a pediatrician in the practice initiated the partnership with UAS, the entire practice now utilizes allergy services for its adult and pediatric patients.
Every year, the practice provides allergy testing and immunotherapy to a steady stream of patients, which also results in a consistent stream of added revenue, typically exceeding six figures annually.
About the Practice
THE PRACTICE: Primary care
PATIENTS: Adults and children
LOCATION: East Coast
SERVICES: Comprehensive primary care in one convenient location
MEDICAL TEAM: 4 physicians and 3 CRNPs
UAS IMPLEMENTATION DATE: May 11, 2015
A Win-Win
Prior to the partnership with UAS, practice physicians referred allergy patients to an outside specialist. Since adding allergy services in-house, the practice has seen:
- The growth of on-site allergy testing
- A reduction in the number of sick visits related to allergies
- Patients who feel more comfortable with testing and immunotherapy due to the convenience and comfort of it being provided in familiar surroundings
- Higher patient compliance with allergy treatment protocols
The practice’s patients now see allergy testing and immunotherapy as an integral part of the services they receive and report that it is more cost-effective than getting the same
care from a specialist. For the practice, offering allergy services helps keep patients within the office for coordinated care.
When asked why the practice chose to partner with UAS instead of providing a home-grown allergy service solution, the Director of Operations offered the following:
“UAS provides comprehensive support in deploying our allergy services. The team provides labor-intensive operation support, such as marketing, employee management, prior authorization, and screening processes. Most importantly, the UAS leadership team provides protocol compliance, quality assurance, and consultation support to ensure that every patient receives the greatest care possible.”
Patient Success Story
Here’s just one patient’s perspective on her experience with UAS after having received allergy injections since July 28, 2023:
“Prior to me taking allergy injections, I was constantly sick, catching colds, bronchitis, all kinds of upper
respiratory infections, and having asthma attacks. Being treated with steroids and antibiotics for the majority of
my life really made me tired.“Finally, at the age of 48, I got sick of being sick and just decided to try immunotherapy. I scheduled my
appointment with our lab, and that is where I met the amazing Clinical Allergy Specialist, Megan. She is a very
confident, knowledgeable, friendly and patient individual. She walked me through the process and made sure to
answer any and all questions or concerns.“Since I have been on allergy injections, my life has changed tremendously. I have not had any major colds or
anything. Even my doctor made a comment when I came in for my physical. She was surprised that she had not
seen me for any sick visits. Thanks to your amazing staff. They are truly making this process a great experience.”
Conclusion
Every practice stakeholder benefits from providing in-house allergy care as an ancillary service. Allergy testing and immunotherapy deliver an additional revenue stream, improve patient outcomes, and free up time for physicians to focus on other health issues due to the support that’s in place for their chronic allergy sufferers.
Patients appreciate the one-stop convenience while receiving high-quality services that help improve their lives. The integration of allergy services has enhanced patient satisfaction and strengthened the practice’s financial stability and potential for growth.
Maximizing Your Practice by Minimizing the Leakage
Does your medical practice have leaks? Is your growth hindered by “lost business” that negates the full impact of new patient growth? One of my favorite business expressions is from Roger Enrico, the former CEO of PepsiCo, who would say: “Growth is what matters.” It was one of the cornerstones that made PepsiCo the evolving company that it is and helped form the company’s distinguishing strategy.
Growth Comes in Many Forms
- Acquiring New Patients
- Raising Prices
- Capturing More of Your Existing Patients’ Healthcare Needs
Real growth comes from acquiring new patients and providing more services to your existing patients. Raising prices, which is not much of an option in today’s insurance reimbursement-dominated world, is often a fool’s errand and not real growth. It may create short-term revenue increases, but, at some point, the economics of supply and demand take over and patients leave for cheaper alternatives.
It is also said that if you are not growing, you are dying. In any business, growth is the pathway to sustainability for the company, its employees and customers. Many businesses have come and gone. Margins decline, investment in marketing and other customer-facing enticements disappear, and the business spirals downward. There are many examples of companies like this: Sears, Kodak, RCA, and Bed Bath and Beyond are just a few. They lost sight of their customers’ needs, and their customers fulfilled those needs elsewhere.
Your practice is a business with similar needs and challenges. There are technologies and services that entice your patients every day, including urgent care, telemedicine, allergy care, spa services, concierge services, and lifestyle services such as hormone replacement and weight loss, to name a few. As your patients seek these services, where will they go? As they are lured away to meet their needs, will they return to you? Will this begin a downward spiral for your practice?
Did you know that a leaky faucet that drips at the rate of one drip per second can waste more than 3,000 gallons per year? That’s the amount of water needed to take more than 180 showers! Small leaks are often ignored, but over time, the impact can be staggering.
Does your practice have leaks? Is your growth hindered by “lost business” that negates the full impact of new patient growth?
Take a Look at Allergy Care Services
A smart way to grow is to find ways to expand your offerings and keep your patients within your practice. What services do your patients need that you can offer? Allergy care can be an easy starting point. Over 50 million Americans suffer from allergies and asthma. These patients can be miserable and often self-medicate to treat symptoms without addressing the underlying cause. In today’s world of rapidfire patient visits with limited time to diagnose, treat and counsel, it is common to refer these patients out for care.
More recently, these patients are being lured by multiple telemedicine options offering easy access to care. Allergy care is a perfect example of a service many of your patients need that you can provide. Nearly one in three U.S. adults and more than one in four U.S. children reported having a seasonal allergy, eczema or food allergy in 2021, according to new data from the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics. Almost 6% of U.S. adults and children have a food allergy, with Black, non-Hispanic adults and children the most likely to report this type of allergy.
50million+
Americans diagnosed with seasonal and environmental allergies
24million
Americans have seasonal allergic rhinitis
3.1million
missed work days per year
Seasonal & Environmental Allergies
Take a look at data revealed in two new reports from the National Health Interview Survey: “Diagnosed Allergic Conditions Among Adults, United States, 2021” and “Diagnosed Allergic Conditions Among Children Aged 0 – 17 Years: United States, 2021.”
Findings from Adult’s Report1
- ABOUT ONE QUARTER (25.7%) OF ADULTS have a seasonal allergy, 7.3% HAVE ECZEMA and 6.2% HAVE A FOOD ALLERGY
- WHITE, NON-HISPANIC ADULTS ARE MORE LIKELY TO HAVE A SEASONAL ALLERGY (28.4%) compared with Black non-Hispanic (24%), Hispanic (18.8%) and Asian non-Hispanic (17.0%) adults
- The percentage of adults with ECZEMA IS HIGHER AMONG WOMEN (8.9%) THAN AMONG MEN (5.7%)
- BLACK NON-HISPANIC ADULTS ARE MORE LIKELY TO HAVE A FOOD ALLERGY (8.5%) compared with Hispanic (4.4%), White non-Hispanic (6.2%), and Asian non-Hispanic (4.5%) adults
Highlights from Children’s Report1
- NEARLY 1 IN 5 CHILDREN (18.9%) HAVE A SEASONAL ALLERGY, 10.8% have eczema and 5.8% have a food allergy
- BOYS (20%) ARE MORE LIKELY TO HAVE A SEASONAL ALLERGY THAN GIRLS (17.7%)
- CHILDREN 6 – 11 YEARS ARE MOST LIKELY TO HAVE ECZEMA (12.1%), followed by children 0 – 5 years (10.4%) and children 12 – 17 years (9.8%)
- BLACK NON-HISPANIC CHILDREN ARE MORE LIKELY TO HAVE A FOOD ALLERGY (7.6%) compared with Hispanic (5%) and White non-Hispanic (5.3%) children
1 Prevalence and Severity of Food Allergies Among US Adults. JAMA Network Open 2019. The Public Health Impact of Parent-Reported Childhood Food Allergies in the United States. Pediatrics 2018. Food Allergy in the United States: Recent Trends and Costs – An Analysis of Private Claims Data. FARE Health White Paper, November 2017.
85%
of asthma patients have allergic rhinitis
50% more
likely to have allergies if one parent has allergies
75% more
likely to have allergies if two parents have allergies
Allergy Care Supports Patient Retention
Where are these patients getting the care that they need today? Rather than risk losing these patients, you can partner with ancillary service providers such as United Allergy Services to offer the highest quality allergy testing and immunotherapy treatments in your office. United Allergy Services brings expertise in areas such as leading immunotherapy protocols, inventory management, clinical support, best practice management, staff recruiting/hiring/training, revenue cycle and more—freeing you and your staff to focus on providing the best clinical care for your patients while generating additional revenue.
As you think about your growth plans for this year, don’t forget to focus on stemming the leakage. It’s there, and it’s real. Let United Allergy Services enhance your practice by helping you extend the care you provide your patients.
Learn more about how UAS can improve your practice and create a patient-centered medical home with comprehensive care.
Why Offer Allergy Treatment for Children?
For providers passionate about providing care to the pediatric population, integrating fundamental allergy care into their practice can bring about significant benefits. Allergy screening, testing, and treatment fosters healthier lives and also enhances the overall quality of care that can be provided.
Allergy immunotherapy, commonly known as allergy shots or allergy drops, is a therapeutic approach designed to modify the immune system’s response to allergens. While regularly considered for adults, recent increased adoption by pediatric providers has paved the way for immunotherapy’s integration into pediatric care, offering a transformative option for managing allergies.
Advantages
One of the primary advantages of incorporating allergy immunotherapy into pediatric care is the potential for long-term relief from allergy symptoms. When children are exposed to small, controlled amounts of the allergens that they are allergic to, their immune system gradually builds tolerance. This can result in reduced severity and frequency of symptoms, decreased allergic reactions, decreased asthma exacerbations, preventing the development of asthma, and less antibiotic and steroid use, as well as leading to a significant improvement in the overall quality of life for pediatric patients.
For many pediatric patients with allergies, the standard approach involves medications to manage symptoms as opposed to foundationally changing the state of the disease. Medication issues can include high cost, unwanted side effects, and only partial control of symptoms. Allergy immunotherapy, however, offers a natural alternative that aims to modify the body’s immune response, substantially reducing or eliminating symptoms, and potentially reducing or eliminating the need for long-term medication use.

Individualized Immunotherapy
Every child is unique, and so are their allergies. Allergy immunotherapy allows for individualized and targeted treatment plans tailored to each child’s specific allergens, lifestyle, and the family’s financial situation. This individualized approach maximizes the potential for efficacy as well as adherence. Also, offering allergy immunotherapy as a pediatric provider creates an opportunity to further strengthen partnerships with parents and caregivers.
Collaborating on a comprehensive treatment plan fosters trust and active involvement in the child’s healthcare journey. It positions pediatric providers as already trusted members of the child’s healthcare team serving as proactive partners in managing and alleviating allergic conditions. This further positions pediatric practices as leaders in proactive and preventive healthcare for children.

How Does UAS Partner with Providers?
How can healthcare providers balance the demands for more patient quality time and the financial requirements for a sustainable practice? Although it may seem counterintuitive to offer an additional service line, doing so can deliver higher revenue, additional clinical support, and meet rising patient care needs.
Consider In-Office Allergy Testing and Treatment
While over 100 million Americans suffer from environmental and food allergies, only a fraction seek treatment from a specialist. This situation creates an opportunity for providers to offer allergy testing and treatment services inside the practice.
United Allergy Services (UAS) partners with providers to significantly enhance the clinical and financial performance of the practice and improve the lives of patients. We expand access to affordable, high-quality allergy care seamlessly delivered in-office, under the direction and supervision of the on-site provider.
How a Partnership Between Providers and UAS Works
UAS offers a range of options for testing and treatment for patients suffering from allergies, including:
- Food Allergy Testing: UAS tests to identify foods that the patient is allergic to and foods the patient may have a sensitivity or intolerance to. We can rule out a potential food allergy with a negative test. Once a patient’s specific allergies are identified, we then provide educational support regarding what foods these allergens can be found in to help the patient develop strategies to avoid them as best practice.
- Environmental Allergy Testing and Treatment: UAS tests for environmental allergies and then treats the patient with immunotherapy that modifies the underlying allergic condition instead of simply treating the symptoms. Immunotherapy is custom formulated from each patient’s allergy test and individual history, developed on-site at the practice. Treatments can be:
- Allergy shots administered in-office or at home by the patient, or
- Allergy Allay Drops® (UAS’s branded sublingual immunotherapy) administered by the patient at home
There are three UAS partnership structures to choose from:
- UAS-Staffed Allergy Center: Fully staffed with a Clinical Allergy Specialist (CAS) and integrated UAS allergy services imbedded within the practice, with all clinical decisions driven by the provider
- Self-Managed Kit Package: Provider practice receives online learning modules, supplies and customer support for everything needed to provide allergy testing and treatment solutions, with existing practice staff providing and managing the allergy services
- Flexible Hybrid Package: Staffing-only solutions:
- UAS hires and manages an allergy technician for practices that have their own allergy protocols but have a difficult time hiring
- UAS can fully train and support the practice’s employee on the UAS protocol and provide the full range of services, systems and support as in the UAS-staffed model
A Win-Win for Providers and Patients
A partnership with UAS enables practices to offer convenient in-house allergy care that improves patient quality of life and satisfaction while generating additional revenue. The practice maintains full clinical control and can easily test, treat and educate patients on environmental and food allergies with comprehensive UAS solutions including practice training, supplies, customer support, patient education tools and marketing materials.
By providing an alternate workstream within the practice, providers can free up their time to attend to other patients who need them while UAS helps take care of the allergy patients.

Why Offer Allergy Care Services in Your Medical Practice?
More than 100 million Americans suffer from environmental, seasonal and perennial allergies, including ragweed, pollen, dust mites and animal dander. In addition, roughly 11% of adults and 7½% of children have a food allergy. Unfortunately, only a fraction seek treatment from a specialist, resulting in an annual cost of $18 billion to the healthcare system and businesses in the U.S.1
Most patients self-medicate with over-the-counter medications, but allergy relief can be elusive. The underlying cause of the condition still goes untreated and leaves patients suffering. The numbers are alarming, as 30% of adults and 40% of children struggle with allergies in the U.S.2
At the same time, providers are getting squeezed between wanting more time for quality patient care and the financial demands that ensure sustainable revenue for the practice.
On-Site Allergy Testing and Treatment
United Allergy Services (UAS) helps by partnering with medical practices to deliver in-office allergy testing for environmental and food allergies. While food allergies are usually dealt with by avoiding the allergen, environmental allergies can be successfully treated via immunotherapy.
Adding this service line improves the lives of patients by expanding access to affordable, high-quality allergy care as a seamless part of the practice and delivers an additional revenue stream to drive financial performance.
Why Immunotherapy?
Allergen-specific immunotherapy has been used to treat environmental allergic issues for over a century. It is the only treatment that addresses the immune dysfunction underlying allergic responses rather than simply treating symptoms or suppressing inflammation. It has been proven safe and effective in treating issues such as allergic rhinitis and asthma and can be offered by a primary care provider without needing to send the patient out to a specialist.3

How Partnering with UAS Works
UAS partners with providers to test patients for allergies in the office and then creates a custom formulated immunotherapy from the patient’s allergy test and individual history. Treatments include:
- Customized immunotherapy based on the patient’s history and test results is formulated onsite under provider supervision
- Allergy shots administered in-office or at home by the patient, or
- Allergy Allay Drops® (UAS’s branded sublingual immunotherapy) administered by the patient at home
UAS delivers a range of options for providers, including:
- UAS-Staffed Allergy Center: Fully staffed and integrated UAS allergy services within the practice itself (with all clinical decisions being driven by the provider)
- Self-Managed Kit Package: Provider practice receives online learning modules, supplies and customer support for everything needed to provide allergy testing and treatment solutions, with existing practice staff providing and managing the allergy services
- Flexible Hybrid Package: Staffing-only solutions
- UAS hires and manages the allergy technician for practices that have their own allergy protocols but have a difficult time hiring
- UAS can fully train and support the practice’s employee on UAS protocol and provide the full range of services, systems and support in the UAS-staffed model but with the practice employee operating as the allergy technician
A Win-Win for Patients and Providers
UAS allergy testing and treatment services are proven, flexible, and customizable. They directly meet the allergy health needs of patients without requiring them to go elsewhere, keeping patients – and their dollars – within the provider’s practice.
Click the button below to learn more about working with UAS to add allergy testing and treatment services to your practice.
1 https://www.webmd.com/allergies/allergy-statistics. Accessed 10.31.23.
2 Ibid. Accessed 10.31.23.
3 https://pubmed.ncbi.nlm.nih.gov/27927826/. Accessed 10.31.23.

Ancillary Medical Services
In today’s world of declining insurance reimbursements and a multitude of competing options for patients to access care, vibrant, healthy practices are constantly seeking opportunities to grow. Growth can come from expanding your patient base as well as expanding your offerings by offering ancillary medical services to your existing patient base and capturing an increasing share of their healthcare spend.
Growing Your Practice with Ancillary Medical Services
Ancillary medical services can set a practice apart from the competition and enhance its ability to better serve patients. When primary care investment increased, both hospital stays and ED visits decreased, as reported by the Patient-Centered Primary Care Collaborative in 2019.
Allergy assessment and treatment, like that provided by United Allergy Services, is an ancillary service that physicians can offer to both serve patient needs and drive additional revenue into the practice.
Three Steps to Determine Whether Ancillary Medical Services Are Right for Your Practice
Before implementing an additional patient service in a medical practice, take these three steps:
- Consider the current state of the practice
- Qualify the ancillary services vendor
- Determine the cost of investment
1. Reflect on the Practice
The first step is evaluating the practice for untapped potential in both the physical space and services offered. What services are your patients seeking elsewhere either by choice or your referral patterns? These services could be services covered by insurance or they could be consumer-based medical services that your patients are exposed to through other care outlets. The advent of internet-based care outlets has greatly expanded the demand for certain services.
Missed Opportunities
A study published in the Journal of the American Board of Family Medicine (JABFM) noted that physicians are often unable to close the referral loop due to lack of referral completion. In fact, 17% of referred patients do not see the specialist to whom they are referred, according to the JABFM study. Is there a needed service in your community that your practice can fill?
Existing Infrastructure
Available space along with current staff productivity levels and credentials impact the practice’s ability to execute additional patient services. Consider how much time and money it would take for staff education and office renovation before a new service line would be functional in the existing practice.
Patient Evaluation
Alignment with patient needs is critical for the success of any ancillary medical service implementation. Consider the areas of common patient referrals, insurance contracts on file that may influence reimbursement rates, and patient perception of the practice.
17%
of referred patients do not see the specialist to whom they are referred
2. Qualify the Ancillary Medical Services Vendor
Patient care should meet or exceed current practice standards. Ask the vendor:
- What additional patient services do they deliver through implementation and beyond?
- What is their track record?
- What sets them apart from their peers?
Resource Leveraging
A valuable partner will offer provisions that boost the likelihood of success when implementing a new service. Look for available customer support expertise in legal regulations and payer reimbursement for the additional patient services you may onboard. When you meet with a prospective vendor, ask about their expectations regarding qualified candidates for their services and reasonable revenue expectations for the practice.
Vendor Reputation
Partnership with an outside vendor requires a high level of trust. Review the vendor’s references and referrals from colleagues as well as their longevity and experience. Vet potential vendors by researching clinical studies that review the company’s protocols.
3. Determine the Cost of Investment
An expansion of services may require additional resources. Consider the financial investment and the potential ROI opportunity after implementation.
Filling a Gap in the Market
Consider whether adding an ancillary medical service to the practice will be profitable. The most popular ancillary medical services adopted by internal and family medicine are lab services, ECG, prescription dispensing, and radiology/imaging. Adding an ancillary service into a market that is saturated may not be a good business decision. While shopping around for service line vendors, consider what unique market gap you can fill that fits your patient base.
Vendor Buy-In
Choose a vendor with infrastructure to handle not only implementation but staffing and ongoing customer assistance. This backing will help lower upfront costs needed for training and reduce the impact on productivity among existing team members.
What Is Your “Return on Effort“?
Your and your staff’s time is a precious resource. Any investment of time and money should generate a sufficient return to justify the expense. Here are a few questions to answer:
- What is the expected demand for the product or service?
- How will you identify potential patients/consumers?
- What is your investment to initiate the service?
- What is your cost to deliver and maintain the service?
- Is this incremental to your practice, or will this replace or cannibalize some of your existing business?
You do not need an MBA to answer these questions. Your vendor and some common sense can help you answer them. Also, your physician community may have experience with the product or service and can help you develop a simple financial model of the potential revenue and costs.
Does It Work?
Adding a service to a practice should be beneficial for patients and improve ROI for the practice. Adding a service to an existing practice has the potential of improving patient adherence and minimizing the need for referrals overall. 70% of polled physician organization leaders noted that increasing the volume of services delivered is the top action that primary care and specialist physicians could take to increase their compensation.
Take a Look at On-Site Allergy Services
Over 100 million Americans suffer from allergies such as rhinitis (hay fever), food allergies and asthma, but only a fraction seek treatment from an allergist. United Allergy Services (UAS) empowers physicians to offer on-site allergy services that fit seamlessly into existing medical office workflows, expanding delivery of patient services and increasing revenue.
Since 2009, UAS has successfully partnered with more than 2,450 practitioners across 20+ states to deliver proven, flexible and customizable ancillary medical services that directly meet the allergy needs of patients without requiring them to go elsewhere. Treatment protocols include immunotherapy delivered by subcutaneous injections (allergy shots) in the physician’s office or at home as well as sublingual allergy drops self-administered at home by the patient. A UAS treatment group showed >40% improvement in allergy symptom scores compared to control through administration of immunotherapy. A 3-year course of immunotherapy has shown long-term clinical effects and the potential of preventing the development of asthma in children with allergic rhino conjunctivitis up to seven years post-treatment.
UAS medical partners maintain full clinical control and can easily test, treat and educate patients on environmental and food allergies with comprehensive solutions that include staff training, supplies, customer support, patient education tools and marketing materials.
The convenience of in-house allergy care both improves patient quality of life and satisfaction while generating additional revenue for the practice.
Am I Suffering from Allergies? Or Something Else?
There is a wide range of variability from person to person when it comes to allergies. The unique circumstances of each person and their environment as well as what type of symptoms occur, how often they occur, and how troublesome they are all have significant meaning.
Gathering this important clinical information is vital to providers as they are trying to determine if allergies may be playing a role. The ability to identify an association between allergic symptoms and allergen exposures is key and sometimes even definitive in deciding to proceed with allergy testing or immunotherapy.
An easy to use, simple to use, and quick-to-complete symptom screening tool is available in allergy clinics offering United Allergy Service’s line of allergy care options. This screening form offers standardization for this critical initial clinical investigation. It offers the opportunity to focus on seven core symptoms that can be strongly indicative of allergic disease.
The screening tool allows providers to assess the presence of symptoms with a strong indication for allergic disease, the frequency of these symptoms, and the presence of other allergic conditions such as atopic dermatitis and asthma. The greater the symptom score, and the more regular or frequent the symptoms occur, the higher the consideration for an allergy skin test should be. Atopic conditions such as atopic dermatitis and asthma, as well as symptom modifying medication use that has failed to control symptoms, also build more strength in the decision to undergo an allergy test.
This screening tool can also help to capture valuable information even after patients are scheduled for or have already had their allergy test. It can help determine the need for allergy testing and possibly immunotherapy, as well as track the decrease in symptoms and the positive impact immunotherapy has had. Completion of this symptom screening form can also help identify an increase in tolerance to a specific allergen that was previously a trigger, any reduction in medications previously used to lessen allergy symptoms, and any additional clinical benefits noted such as a reduction in asthma exacerbations, sinus infections, ear infections, or dermatitis.
If you feel you may be suffering from allergies, we encourage screening utilizing an allergy symptom screening tool like the one available in UAS allergy clinics or the online allergy quiz available on our website. It’s a great way to start your journey of improving allergy symptoms and your quality of life!
Summer Allergies
What do you look forward to in the summer months? I bet it isn't summer allergies! Whether you are planning to be the grill master or the ultimate host of the patio celebration, we have tips to help you prepare. Today, let’s discuss some common summer allergens you may encounter when enjoying the sun or attending summer celebrations.
During the summer months, many allergy sufferers are wary of grass pollen. They are the most common seasonal allergy triggers and are heaviest in May through August. Don't forget to check local pollen counts to determine the density of pollen in the air on any given day. Read more about Grass Pollen Allergies and avoidance tip in our blog post here.
Skin Reactions
With many summer celebrations occurring outside or around the pool, sunscreen is important to discuss. We all know sunscreen is a crucial part of summer safety, but sometimes it can cause a reaction much worse than a sunburn. Individuals can have a contact allergy to the sunscreen itself and a rash will appear where it was applied. A reaction that appears after applying the sunblock and being exposed to the sun is also possible. Apply a quick and simple patch test before applying the product to your whole body. Decide on a small area like the wrist, apply the product, and wait at least 24 hours to make sure the skin does not react.
Also, while chlorine isn't an allergen, it is an irritant and can cause problems with eye and nose itching. It can also cause breathing problems in people with asthma. If undesired symptoms are occurring while swimming, jump out of the pool. Take off your suit and wash the affected area with clean water and soap to remove traces of the remaining irritant. It is a good idea to have a rescue inhaler on hand, if prescribed to you, to calm any respiratory symptoms should they occur.
Stinging Insects
Stinging insects such as bees, wasps, hornets, and yellowjackets are most active during summer and early fall. Also fire ants are active all year round in many southern parts of the United States. People who know they are at risk for an allergic reaction to stinging insects should always carry two doses of auto injectable epinephrine. It is important to have the ability to access the injections within 60 seconds if necessary. Try to avoid the stings and bites before they occur by refraining from walking outdoors barefoot, especially in grassy areas. Skipping perfume or sweet-smelling body sprays or lotions is another good avoidance technique. Also, do not drink out of cans or bottles that have sat open and unattended. Sometimes insects can get trapped inside. Finally, when choosing the perfect outfit for the holiday weekend’s plans, leave any vivid, floral clothes in the closest.
Asthma Concerns
Fireworks, although beautiful and breathtaking, can create smoke and small particulate matter can trigger asthma. If you suffer from asthma, consider watching the fireworks from an indoor location. Similar to fireworks, smoke from grills, bonfires, firepits, or outdoor fireplaces can also trigger asthma. Try to avoid the direct smoke pathway, leave significant distance between yourself and the source of the smoke, Finally, other scented products utilized during outdoor gatherings can also contribute to air pollution and can trigger asthma. If hosting a party, contact your guests and ask if certain things like scented insect repelling candles or torch oil trigger negative responses for them.
Finally, what would a summer celebration be without all the tasty food and drinks? If food allergies are present, it may be easier to pack your own meals or snacks to have readily available. Preparing food yourself is always the safest option. If it isn't feasible to do so, you still have options. It is helpful as a host to ask about any food allergies or dietary restrictions when inviting guests to the event. It is also very helpful to label what individual dishes or offerings are and include a high-level recipe or ingredient list. That way guests can privately identify safe selections off the menu and enjoy immersing themselves in the full experience without the worry of unknown exposure.
Amanda Hofmann, MPAS, PA-C, is a graduate of Duquesne University, in Pittsburgh, Pennsylvania. After spending eight years in clinical practice, she joined United Allergy Services as the vice president of clinical. Amanda is also the past president of the Association of PAs in Allergy, Asthma, and Immunology.
United Allergy Services is also on Facebook, LinkedIn, or Twitter. See other interesting and related articles on the UAS Blog.
Eosinophilic Esophagitis (EoE)
Eosinophilic esophagitis (EoE) is a recognized diagnosis that produces symptoms related to dysfunction of the esophagus. In EoE, large amounts of white blood cells, specifically eosinophils, collect in the inner lining of the esophagus resulting in inflammation. Typically, the esophagus is free from eosinophils and resulting inflammation, and so in EoE, a patient will begin to notice a difference in the way they can eat and swallow food. This condition can be difficult to diagnose as other conditions can present with eosinophils in the esophagus, and historically EoE has not been a common or well-known disease. Awareness has significantly improved however in the last decade, and patients are being recognized and diagnosed much earlier. This week, the FDA has approved the first ever treatment for EoE.
Symptoms of EoE
Many EoE patients also have symptoms of one or more allergic disorders like asthma, allergic rhinitis, atopic dermatitis (eczema) and food allergy. It is important for EoE patients to be properly assessed and tested for potential allergens as well as properly diagnosed for their atopic conditions. Similar to proper diagnosis, it is crucial that any and all allergic aspects of EoE can be properly treated in conjunction with management of the EoE. Patients benefit from a team of providers working together such as a primary care provider, allergy specialist, and gastroenterology specialist.
Early diagnosis of this chronic condition is important so patients can be educated and properly managed, sparing them from discomfort, malnutrition, and even life-threatening situations. An emergent situation can arise if inflammation becomes too great and causes narrowing in the esophagus, trapping swallowed food. In younger children, EoE typically presents with poor feeding, failure to grow properly, vomiting, reflux symptoms, and abdominal pain, whereas in adolescents and adults EoE most often presents with dysphagia (trouble or painful swallowing) and emergent esophageal food impactions.
Allergy Correlation
Airborne allergies can play a role, however adverse immune responses to food are the main cause of EoE in many patients. It can be more difficult to properly diagnose food allergies in EoE patients because many do not present with the typical symptoms associated with IgE mediated food allergy. Instead of immediate itching, flushing, hives and vomiting after ingestion of the offending food, the reactions can be delayed over hours or days. Milk, egg, soy and wheat are recognized as the most common triggers for EoE, however, conventional allergy tests often fail to detect sensitivity to the foods causing EoE. This is because most food allergy reactions in EoE are delayed and caused primarily by immune mechanisms other than classical IgE-mediated food allergy.
Diagnosis
Other than proper identification and diagnosis of atopic conditions, EoE must also be properly diagnosed itself as a disease. If EoE is suspected, a specialist performs an upper endoscopy, where a small tube with embedded camera is passed down the esophagus. The tube not only has a camera and light for inspection, but a small device to take samples, or biopsies of the esophagus. The biopsies of the esophagus are examined under a microscope for eosinophils and inflammation and are necessary to diagnose EoE. A provider looks for appropriate symptoms that were described above, visual inspection of the esophagus, and examination of tissue biopsies to make the final diagnosis of EoE.
Managing EoE
There are many viable options to managing EoE effectively. Food sensitivities or allergies can be managed by removing those offending foods from a person’s diet, but only under the direct guidance and supervision of a provider. A provider can advise eliminating a specific food, or a food group based on individual history, examination, and diagnosis. This elimination approach can be helpful to some, but it is important to only remove what is advised, and a medical provider will closely monitor a person and regularly discuss nutrition and intake. Many times, a dietician is added to the medical care team to make sure a person is still receiving all the necessary nutrients. A provider’s goal is to carefully add back any foods that can in fact be tolerated and are proven not to incite eosinophils in the esophagus.
Aside from adjustments to a person’s diet, there are some medications providers use to help provide symptom relief and management of the EoE. It is important to note that aside from the first medication being approved by the U.S. Food and Drug Administration (FDA) to treat EoE, typical options for treatment include proton pump inhibitors and steroids. Proton pump inhibitors (PPIs) reduce acid production in the stomach and have also been found to be able to reduce esophageal inflammation in some patients with EoE. PPIs are very commonly used as a frontline therapeutic for EoE patients. If PPIs do not work for a patient, another option may be swallowed topical corticosteroids. Swallowing small prescribed doses of corticosteroids so they come in direct contact with and treat the inner lining of the esophagus is the most common treatment.
Amanda Hofmann, MPAS, PA-C, is a graduate of Duquesne University, in Pittsburgh, Pennsylvania. After spending eight years in clinical practice, she joined United Allergy Services as the vice president of clinical. Amanda is also the past president of the Association of PAs in Allergy, Asthma, and Immunology.
United Allergy Services is also on Facebook, LinkedIn, or Twitter. See other interesting and related articles on the UAS Blog.
Allergies, Asthma, and Air Quality
As we move into the summer months, it is important to understand the connection between allergies, asthma, and air quality. While air pollution does not directly cause allergy or asthma, it can increase the risk of developing atopic disease. Air pollution can also trigger allergy or asthma symptoms or an asthma attack for persons with existing conditions. Air pollution usually increases during summer months. This pollution leads to an increase in related symptoms, urgent office visits, and emergency room visits.
Air Quality Components
Allergy and asthma symptoms can be triggered by two key air pollutants, ozone (found in smog) and particle pollution (found in haze, smoke, and dust).
- Ozone, a gas, is one of the most common air pollutants, contributes to smog, and is more common in cities where there are a lot of cars. In the summer months ozone can increase when intense sunlight and heat convert a mixture of tailpipe and power plant emissions with other chemicals resulting in unhealthy air. Allergy and asthma symptoms may trigger more easily because ozone is irritating to the lungs and can reduce lung function.
- Particle pollution is present and stable throughout the year but is typically worse near busy roads, during rush hour and around factories. It is also high when there is smoke in the air from wood stoves, fireplaces, or burning vegetation. These small particles can irritate the nose, throat, and especially the lungs, and also reduce lung function and cause asthma exacerbations.
Air Quality Reports
The United States Environmental Protection Agency (EPA) reports air pollution levels using the Air Quality Index (AQI). AQI reports the level of ozone and other air pollutants. When the AQI is 101 or higher, it is dangerous for people with allergies and especially asthma. Sometimes asthmatics can experience increased symptoms even when ozone levels are moderate (AQI 51-100). Many local news stations and weather forecasters report local air quality to advise the public about moderate or high pollution days.
Another resource, The American Lung Association has just released their annual State of the Air report. One interesting finding in the report is, “The addition of 2020 data to the 2022 “State of the Air” report gives a first look at air quality trends during the COVID-19 pandemic. Regardless of the shutdowns in early 2020, there was no obvious improvement.”
Combatting Air Quality Conditions
When air quality may be dangerous to people with allergies or especially asthma, they are deemed as “Action Days”. During Action Days, people with asthma should limit their time outdoors, especially in the afternoon or rush hour periods, stay in a well-ventilated, preferably air-conditioned, building, and most of all, do not intensely exercise outdoors. Also try to keep windows closed in your home and car, and instead utilize the air conditioning on the recycled setting.
There is also a risk that you could have poor indoor air quality within your home. Irritants can exacerbate allergy and asthma symptoms. These and allergy and asthma triggers are common items such as:
- household cleaners
- hair products
- perfumes
- air freshening sprays or plug ins
- scented candles/diffusers
- smoke produced from
- tobacco
- fireplaces
- candles
- cooking
- wood burning stoves
Not smoking or permitting smoking in the home is one of the easiest ways to protect the home from indoor air pollution. Finally, be mindful of high humidity and mold growth. These two factors can greatly impact indoor air quality. Installing exhaust fans in kitchens, bathrooms, and laundry rooms can help lower humidity. The use of a dehumidifier helps significantly as well.
Amanda Hofmann, MPAS, PA-C, is a graduate of Duquesne University, in Pittsburgh, Pennsylvania. After spending eight years in clinical practice, she joined United Allergy Services as the vice president of clinical. Amanda is also the past president of the Association of PAs in Allergy, Asthma, and Immunology.
United Allergy Services is also on Facebook, LinkedIn, or Twitter. See other interesting and related articles on the UAS Blog.
Earth Day and Climate Change Effects
Earth Day is this Friday, April 22nd. Earth Day is truly a mainstay in American culture, created by Past-President Richard Nixon. This year the Earth Day theme is “Invest in Our Planet”. We are called upon to have “unstoppable courage to preserve and protect our health, our families, our livelihoods…” One of the continued focal points of interest is trying to put a dent in rising global temperatures, with an average increase of 2.4 degrees Fahrenheit in the last 50 years. It doesn’t sound like a lot, but each degree brings bigger changes than many realize. The rising temperatures have a directly negative impact on allergy sufferers and those offering optimal allergy care to their patients.
Effects on the Planet
Warming temperatures results in longer growing seasons. Although people tend to enjoy nature’s natural beauty a bit longer, and farmers have additional time to harvest crops, the increase in temperatures prolong and worsen the suffering of those with pollen allergies and can cause an imbalance in the optimal growth range for crops and cause foods shortages.
Different plants require different conditions to grow, and when the climate continually changes, so do the arrangements and floristic zones of the world’s plants. As the planet warms, we continue to see the planting zones where these plants grow will continue shifting north. Shifting planting zones threaten things like accurate allergy testing panels, cocoa beans for chocolate producers, coffee beans, and maple syrup. Plant species, being entirely mobile beings, will be forced to move upslope or downslope, or species with arrange themselves in new combinations entirely. Finally, the rising temperatures also negatively impact plants by impacting the pollinators that assist with their growth. Warmer temperatures and changing climates have negative effects on pollinator species like butterflies and honeybees. This further shift growing and blooming seasons and further weakens the plant populations.
Allergy Amplification
As the planet warms, allergy season tends to begin earlier and last longer each year. Talk to your primary care provider about allergy testing and treatment options if you notice that your allergies are worsening. You may be a great candidate for immunotherapy, a solution to change the source of your allergy misery rather than treating just the symptoms.
Amanda Hofmann, MPAS, PA-C, is a graduate of Duquesne University, in Pittsburgh, Pennsylvania. After spending eight years in clinical practice, she joined United Allergy Services as the vice president of clinical. Amanda is also the past president of the Association of PAs in Allergy, Asthma, and Immunology.
United Allergy Services is also on Facebook, LinkedIn, or Twitter. See other interesting and related articles on the UAS Blog.
Botanical Sexism: Does it impact allergy sufferers?
What is Botanical Sexism? Tom Ogren, horticulturist and allergy researcher, has done extensive research on ways to reduce pollen counts and pollen potency. His theory centers around the unbalanced planting of male vs female plants. This unbalance can impact pollen counts and the resulting escalation of pollen allergies. He wrote and published an article in Scientific American, coining “botanical sexism” to explain his theory. Ogren believes a better mix or “gender balance” of male and female trees, especially in urban settings, would lower pollen counts.
Ogren’s article focuses on the foundation set in the 1949 USDA Yearbook of Agriculture which reads, “When used for street plantings, only male trees should be selected, to avoid the nuisance from the cottony seed.” This idea comes from the fact that male trees produce pollen, and female trees receive that pollen and produce fruit and seeds. It was recommended to plants primarily or all male tress to avoid messy sidewalks and parks from the flowering female trees that would drop their seeds and fruits.
Tree System Selection
Is botanical sexism a natural selection? Trees have four primary sexual systems: cosexual, monoecious, dioecious and polygamous. A tree that produces single flowers with combined fully functional male and female parts
is called cosexual. Monoecious trees similarly have both male and female parts within the same tree, however they separate the male and female parts into different flowers or cones on the same tree. Dioecious trees separate male and female parts on completely different trees where one tree is strictly female and one strictly male. These trees were Ogren’s primary focus. And for completeness we will define polygamous trees as the most complex and as cosexual, with male and female flowers on the same tree but also with separate male and female parts in different combinations on completely different trees.
Ogren’s work focuses on dioecious males planted independently of dioecious females. This is often the case in urban areas due to the cleanliness concern described above. When this occurs however, their pollen is unchecked by any capture by female flowers and causing copious amount of pollen to be distributed in the air to cause coughing, sneezing, and respiratory issues. Tree pollen is one of the greatest offenders of not only allergic rhinitis, but also allergic conjunctivitis and allergic asthma as well.
Pollen Count Impact
Botanical sexism referenced higher pollen counts due to failed tree “gender balance”, and is further exacerbated by higher pollen potency. Studies have shown that air pollution (which tends to be higher in urban settings) attaches to pollen grains and causes the powdery substance to shatter into still tinier pieces. “When that happens the inside of the pollen grain is exposed and that’s 10 times more allergenic than the outside,” explained Ogren. This is again exacerbated by increasing CO2 levels which causes plants to bloom at a faster rate and at a higher content which means even higher pollen counts where predominantly male trees reside.
Purpose of Defining Botanical Sexism
Prime allergy season is usually defined as mid-March to early June in most of the United States. Frequency of allergic rhinitis (AR) diagnosis increase greatly during this season. AR affects more than 400 million people worldwide, and is expected to rise by another 100 million by 2025. Ogren collected extensive data, and by 2000 was able to develop a scale called OPALS (Ogren Plant Allergy Scale) that ranks more than 3,000 plants from 1 to 10 based on how allergenic they are. This was the first numerical ranking system in existence for plant allergies and is used to develop allergy rankings in large US cities.
Ogren’s work is meant to encourage city planners, plant distributors, and homeowners to think carefully about their plant choices. He feels we all are all responsible for the rising numbers of allergy sufferers, and we, by making the correct plant choices, can at least reduce the amount of allergenic pollen in the air. Examples of plants that are allergy-friendly include pansies, impatiens and snapdragons.
Amanda Hofmann, MPAS, PA-C, is a graduate of Duquesne University, in Pittsburgh, Pennsylvania. After spending eight years in clinical practice, she joined United Allergy Services as the vice president of clinical. Amanda is also the past president of the Association of PAs in Allergy, Asthma, and Immunology.
United Allergy Services is also on Facebook, LinkedIn, or Twitter. See other interesting and related articles on the UAS Blog.
Ragweed and Fall Pollen Allergies
Back to school season is here! Shorter days, crisp, cool evenings, and beautiful fall foliage are on the horizon. This time also marks the onset of weed pollination and the resurgence of allergy symptoms that may have taken a vacation in the hot, dry July heat. The meteorological calendar says fall begins September 22nd, but weed pollen, the main culprit of the sniffles and sneezes during fall allergy season, is already here!
Pollen Offenders
Towards the close of summer, weeds start to pollinate. Weeds grow all summer, but their pollen is usually not released until later in the growing season. This can vary year to year but typically starts mid to late August. Ragweed, cocklebur, lamb’s quarters, pigweed, dock sorrel, English plantain, and sagebrush can all cause fall allergy symptoms and are widely spread across the U.S.
Specifically ragweed pollen is the predominate culprit of allergy symptoms from August through October, peaking on average in mid-September. Ragweed is one of the major drivers of allergy symptoms and releases huge amounts of pollen each and every day. The pollen produced by ragweed is small and light. It is released in large quantities into the air and carried for miles by the wind. Nasal congestion, runny nose, and itchy eyes are typically caused by wind-blown pollen which is easily spread for miles and miles.
Other Pollen Types
Goldenrod, which blooms at the same time that ragweed does, is instead insect-pollinated and therefore is not a significant allergen for most individuals. Insect carried pollen is produced by plants that have bright and attractive flowers. This kind of pollen is typically large and heavy, sticks to insects, and is transported during flight fertilizing other plants. These bright flowers are commonly thought to be allergy offenders, however because they do not release much pollen into the air they are not as likely the culprit of allergy symptoms.

Manage Symptoms
Checking local pollen counts is helpful to anticipate the level of exposure on any given day. Pollen counts are determined by collecting pollen on special rods. The pollen is then counted under a microscope and calculated in grains per cubic meter of air. Pollen counts tend to be the highest early in the day, or often when the wind picks up just before a large rainstorm. If you like dancing in the fall rain, or jumping in rain puddles, however, you are in luck. During a rainstorm and immediately following, pollen becomes still and dormant because the rain makes it damp and heavy. As the air becomes warmer and drier following the storm, however, the pollen count will rise again.
Pollen Avoidance
Those with weed pollen allergies should try to avoid heavily dense wooded areas or those with brush and shrubbery. These areas should be especially avoided in late August when pollen is the most dense and abundant. Pollen counts are never zero, nor will an allergy sufferer truly be able to avoid weed pollen in the late summer and early fall. However, contact may be lessened by taking simple steps to avoid pollen overload:
- Utilizing the air conditioner or heater
- Keeping the windows and doors at home and in the car closed
- Utilizing the dryer rather than the fresh breeze to dry clothing
- Changing clothes after coming in from being outdoors
- Shower prior to getting into bed or laying on upholstered furniture
These easy steps will help to decrease pollen exposures. Also, one benefit COVID-19 may bring allergy sufferers, is that wearing of some masks will help to minimize the amount of pollen reaching the nasal passages if being worn in outdoor settings.
Get Tested
If someone is unsure whether weed pollen is a trigger for their back-to-school nasal congestion, runny nose, post nasal drip, sneezing, and itchy watery eyes, taking an allergy quiz or seeing their provider for an allergy test may provide the clarity they are looking for!
Amanda Hofmann, MPAS, PA-C, is a graduate of Duquesne University, in Pittsburgh, Pennsylvania. After spending eight years in clinical practice, she joined United Allergy Services as the vice president of clinical. Amanda is also the past president of the Association of PAs in Allergy, Asthma, and Immunology.
United Allergy Services is also on Facebook, LinkedIn, or Twitter. See other interesting and related articles on the UAS Blog.
Summer Allergy Travel Tips
School is out, summer is in full swing, and it is prime time for summer vacations and traveling. Summer travel with environmental allergies, asthma, or food allergies may make planning a vacation seem like a daunting task. Not to worry! We can show how to keep summer allergy issues at bay during your staycation, beach trip or wine tour of your dreams.
Summer can be an ideal time to travel. The hot summer months can actually provide relief to some, like those with tree pollen allergies. Unfortunately for others, summer comes with its own allergy triggers. While tree pollen counts tend to be lower, the summer heat pushes grass and mold pollen to be higher. Ragweed begins to appear in the late summer and early fall months to kick off fall allergies. Pollen is not the only trigger you can expect; more stinging insects and hotter temperatures in summer months can complicate matters for asthma sufferers.
Summer Allergy Location Tips

Location is everything! One consideration is that pollen counts tend to be lower on the coast, so beaches may be a good option. The desert, or alternatively snowy mountain tops, can also be ideal for pollen, although maybe not for summer travel. Does your vacation involve hiking or mountain climbing? Dust mites do not prefer elevations above 2,500 feet, so that may be a great choice as well. Wherever you decide to go check the allergen forecasts for that area. You should also check current pollen counts each day there. If high pollen counts are in the forecast, consider planning inside activities during your trip.
Checking pollen counts may not be the only forecast to make sure to monitor. As the temperatures rise, you can expect the humidity to rise as well. Many who suffer from asthma can find their condition aggravated by the high temperatures and humid climate. When planning your time outside during the summer, check the air quality for low humidity and low ozone days. You can also avoid triggers by planning around the heat of the day when possible.
Packing for Vacation
Although your favorite swimsuit may be more fun, allergy control measures should equally be at the highest priority. Staying compliant to your recommended treatment protocol in the days before you leave is crucial. These measures will support well-maintained symptoms while traveling, and for the duration of the trip.
- Make sure to pack allergy medication and immunotherapy in a carry-on bag if traveling by plane.
- Try to keep medications in original packaging and pack all medication and allergen immunotherapy in a separate, clear bag.
- Any liquid or gel medications or immunotherapy will need to individually be 3-4 ounces or smaller. Consider purchasing travel sizes if standard sizes do not meet this requirement.
- Pack 1-2 days of additional medication or immunotherapy than what will be needed in case of delay when traveling.
- It may be beneficial to set a reoccurring alarm on a phone before leaving. Normal routines may change with travel and vacation plans.
- Finally, are you traveling out of the country? If you are traveling to a non-English speaking location, bring a list of your allergies in the native language. You may also learn to say or write “I’m allergic to _____.” in the local language.
Additionally, do not forget to pack any hypoallergenic hygiene products that you regularly use. Examples might be sunscreen, after sun cream, lotions, ointments, body wash, or laundry detergent. When searching for accommodations, remember that more and more hotels offer items like mattress and pillow covers or hypoallergenic linens so you may not have to pack your own. It may also be helpful to ask about smoke free rooms, away from humid, mold friendly pool areas if possible. If pet dander is a concern, take note of whether the location is “pet friendly”.
Summer Allergy Avoidance Tips
Air in enclosed spaces such as planes and trains can sometimes be extremely dry. Consider investing in nasal saline spray or washes, as well as portable humidifier. A humidifier will likely also be beneficial if staying in a hotel for more than a night or two. Staying well hydrated with water and non-caffeinated beverages will also greatly help you combat drying out. If traveling by car, considering utilizing the heat or air conditioning and keeping windows closed. Also, turning on the heat or air 10 minutes before departure can help clear vents of any residual allergen particles.
While enjoying your destination, remember that peak pollen times are typically early in the day (specifically 5am 10am). Scheduling desired outdoor activities for later in the day or just before dusk may help to reduce exposures. Similarly to when you are home, a daily shower is helpful for allergen avoidance. Showering before bed will help to wash away allergens that have adhered themselves to your skin or hair. This is especially important to maintain so that your pillow, sheets, and the immediate space you breathe in all night is allergen free.
Insect Allergies
Another aspect of the summer allergy concerns may be insects. If stinging insect allergies are present planning ahead can alleviate a lot of anxiety and allow for a smooth trip. Always make sure to carry a minimum of two epinephrine auto injectors if it has been prescribed to you or a loved one. Make sure the epinephrine autoinjector is carried in a way it can be accessed and administered within 60 seconds of a need arising.
If you or a loved one does have life threatening allergies, it is a good idea to check with your health insurance and ensure you know where to seek medical care should the need arise while you are out of town. You may also consider carrying an allergy identification card. It can be helpful to keep a card in your wallet listing your allergies, and also emergency contact information and your healthcare provider information. This can be especially important for children who may be summer camps or staying overnight with friends or family.
Food Allergies
If food allergies are present, packing your own meals or snacks may make traveling easier. Preparing food yourself is always the safest option. Alternatively, research the local dining hot spots you wish to visit in advance of leaving for your trip. This allows you to identify safe selections from the menu or you can call to request proper menu accommodations. You may still consider packing your own snacks if you have food allergies. While it may be possible to plan meals around food allergies, snacks often present more of a challenge. Pack allergy friendly snacks, especially if lengthy plane rides are involved.
Amanda Hofmann, MPAS, PA-C, is a graduate of Duquesne University, in Pittsburgh, Pennsylvania. After spending eight years in clinical practice, she joined United Allergy Services as the vice president of clinical. Amanda is also the past president of the Association of PAs in Allergy, Asthma, and Immunology.
United Allergy Services is also on Facebook, LinkedIn, or Twitter. See other interesting and related articles on the UAS Blog.
Tips for Balancing Baseball and Allergies
Spring means longer days, warmer weather, and the beginnings of baseball! Unfortunately for some allergy sufferers, the start of the long-anticipated baseball season also means the time of year when allergens such as tree pollen are at an all-time high. Sneezing, wheezing, and itchy, watery eyes can make games or practice challenging for you or your little leaguer. Even more concerning? The thought of major league games and contact with baseball’s favorite sidekick...peanuts! You can still enjoy this spring and baseball season with a little planning for your allergies.
Eliminating all outdoor sports and activities may seem like the best decision, and for many, it is. However, if skipping out on baseball or other outdoor sports due to allergies just is not an option, we can help. Here are some tips that will help allergy suffers enjoy watching America’s pastime and PLAY BALL!
Airborne Allergy Tips
Check the weather forecast before heading to the game. When checking out the weather, it is good practice to also check the pollen counts in the area. Keep in mind that peak pollen times are typically in the first half of the day, specifically 5am 10am. Attending practices or games midday or in the afternoon may help to reduce exposures.
Baseball and outdoor allergies don't have to be in competition with one another. If you have a little leaguer, packing wet wipes is good practice. Wiping down their hands, face and neck can be helpful to combat those distracting allergy symptoms when out on the diamond. Also, make sure your favorite player is not relying on allergy medication that could make them drowsy. There are non-sedating medication options, or allergen immunotherapy that are worth discussing with their provider.
After a long practice or game, it is beneficial to change your clothing as soon as possible. Also helpful is an immediate shower, especially before crawling into bed. The shower will help to wash away any allergens that have adhered themselves to your skin or hair. This is especially important so that the allergens aren't transferred to your pillow or sheets, remaining in the immediate space you breathe in all night.
Planning for Stinging Insects and Food Allergies
If your allergies include stinging insects or even food, planning ahead can alleviate a lot of anxiety. Always make sure to carry a minimum of two epinephrine auto injectors if there is a known insect or food allergy. Make sure the epinephrine auto injectors can be accessed and administered within 60 seconds if the need arises.
If food allergies are present, especially peanut, legume, or tree nut, it can make the lyrics “Buy me some peanuts and Cracker Jacks” send shivers down your spine. Fortunately, most large baseball stadiums across the country have become aware of the dangers and distress surrounding food allergies and have started to offer peanut-free games or special accommodations for food allergy families with peanut-free designated seating. The Food Allergy Research and Education (FARE) organization typically releases an annual guide outlining which major league and minor league baseball stadiums offer peanut aware sporting events. Along with utilizing their helpful guide, FARE recommends “to reach out directly to the venue to learn more about their efforts”.
Some suggested questions to have ready when you contact the venue about are:
- Are there any [peanut] allergy friendly games, sections, or suites available?
- Does the venue utilize power washing for seating, and traffic pathways at the stadium?
- Can you find ingredient lists or are they available upon request at the concessions?
- Do they allow families to bring in their own safe meals and snacks?
- Are emergency responders available to the public at every game, and are their sections closer to these personnel?
Planning and communication are key to enjoying baseball season and balancing your outdoor allergies. Talk to family, friends, coaches, players, and venues, to create a plan that is right for your family. However, missing out on baseball season does not have to be part of that plan. If you or your loved ones are not quite sure if allergies are playing a role, or if the over-the-counter allergy medication just is not cutting it, you have options. There is still time to see your provider and discuss allergy testing and begin allergen immunotherapy.
About the Author
Amanda Hofmann, MPAS, PA-C, is a graduate of Duquesne University, in Pittsburgh, Pennsylvania. After spending eight years in clinical practice, she joined United Allergy Services as the vice president of clinical. Amanda is also the past president of the Association of PAs in Allergy, Asthma, and Immunology.
United Allergy Services is also on Facebook, LinkedIn, or Twitter. See other interesting and related articles on the UAS Blog.
The Gross Truth About How Often You Should Replace Your Pillow
The Question: How Often Should I Replace My Pillow?
The Answer:
Nearly 70 percent of people say a comfortable pillow is very important to a good night's sleep, but many of us make a crucial mistake when it comes to our favorite pillows: We’re keeping them for way too long.
5 Surprising Ways Hotels Can Make You Sick
When traveling, your hotel is your home away from home. But you and your family may have unwanted company -- your hotel room could be a haven for germs, parasites, and other threats to healthy travel.
Before you book your next getaway, know what dangers could be lurking in hotel rooms and how to avoid travel sickness.
Poor Air Quality
Sub-par air quality in your hotel room can quickly put a damper on your trip and increase the chances that you’ll get sick.
“Stale air is unhealthy. It invites irritants into the body,” says Gaylen Kelton, MD, professor of clinical family medicine at the Indiana University School of Medicine and IU Travel Medicine in Indianapolis. “It can aggravate allergies and just be a nuisance.”
Cigarette smoke is a common irritant. Most hotels in North America offer the option of non-smoking rooms, but they may be harder to find internationally.
“In China, even though there are no-smoking signs on the walls in the hotel rooms, they still reek of smoke,” says Dr. Kelton.
If you do smell smoke or stale air, Kelton says it’s best to resist the urge to turn on the fan or air conditioner. If the air filters aren’t changed regularly, you could make matters worse and blow more irritants into your hotel room. Instead, open a window to get some fresh air into the room.
Germs in Unexpected Places
Most people expect to find germs on places like door handles and toilets in a public place like a hotel. But research shows the highest concentrations of germs in hotel rooms are often in places many people don’t hesitate to touch as soon as they set their bags down.
A small study of nine hotel rooms presented at the American Society for Microbiology in 2012 showed remote controls, telephones, carpets, and bedside lamp switches contained high levels of fecal and aerobic bacteria. Those types of bacteria could lead to gastrointestinal illnesses, among others.
Researchers found that cleaning items on maids’ carts, like mops and sponges, also had high levels of both types of bacteria. That raises the risk of spreading potentially disease-causing germs from room to room while cleaning.
To prevent hotel room germs from spoiling your trip, bring sanitizing wipes and wipe down high contact surfaces when you arrive. Also remember to wash hands frequently.
Slipping Risks
Germs may actually be the least of your worries in a hotel room bathroom, says Kelton. Bigger threats to healthy travel are slips and falls on unfamiliar territory. “More accidents happen in showers from falls than anything else when traveling,” says Kelton.
In hotel room bathrooms, you may encounter a different setup than you're used to at home, and that can trigger falls, says Kelton. For example, you might have a walk-in shower at home, but at the hotel, you have to step into a tub shower. Or the floor may not have a mat or carpet and could become slippery when wet.
Another often-overlooked danger in the bathroom is scalds and burns. “Hotels have the hot water set at a higher temperature than at home, so you need to gauge the temperature appropriately,” says Kelton. “Kids may turn on the hot water all the way at home and be okay, but the hotel’s water is hotter.”
A final water warning for international travelers: Kelton says that if you aren’t going to drink tap water anywhere else on your trip, don’t do it at the hotel either. That means using bottled water to drink in your room as well as to brush your teeth.
Allergies and Sensitivities
Dust mites, down comforters, and other potential allergens might trigger the sniffles in particularly sensitive travelers — allergy and asthma sufferers, we mean you.
If you have allergies or sensitive skin, Kelton says it’s worth calling ahead to ask if the hotel offers allergy-friendly rooms or if they can tell you what cleaning products they use — harsh cleaning solutions or laundry detergents can also be irritating if you have sensitive skin. Some hotel chains will also allow you to pre-order foam rather than feather pillows.
Kelton also advises against trying the tempting free toiletries at hotels if you have sensitive skin. “Using a new soap or shampoo may cause some people to have a reaction,” he says.
Bed Bugs
What's most surprising about bed bug infestations is that they're still a problem. Since the late 1990s, they've had a worldwide resurgence. Bed bug infestations have now been reported in all 50 U.S. states, often in hotels.
The blood-sucking insects feed on people. Bed bug bites can start out as small pricks in the skin, but can grow and become inflamed and cause itching.
More than 40 disease-causing pathogens have been detected in bed bugs, but the good news so far is that there's no definitive evidence that they transmit any disease to humans.
To reduce your risk of becoming a bed bug’s dinner or means of transport to its next meal, follow these steps:
- Check the mattress, box spring, and behind the headboard for signs of bed bugs. Signs may include brown spots (which could be the bugs’ feces) and bed bug skins, as well as any live bed bugs. The bugs tend to harbor in mattress piping.
- Do not put your luggage or other personal items on beds or other soft, upholstered furnishings that may harbor bed bugs. Put clothing and luggage on dressers or luggage racks.
- Keep your suitcases, briefcases, and computers and their cases closed when not in use.
Taking these precautions involves some legwork (and detective work), but it all translates to a better travel experience.
###
By Jennifer Warner
Medically reviewed by Pat F. Bass III, MD, MPH
October 24, 2013
everydayhealth.com